Anticoagulants are a cornerstone in modern medicine, playing a vital role in preventing and treating blood clots. Understanding their working principle is essential for healthcare professionals and patients alike. This blog delves into the science behind anticoagulants, their types, mechanisms, and applications, providing a comprehensive guide to their role in medical practice.
Table of Contents
- 1 Introduction to Anticoagulants
- 2 Principle of Anticoagulants
- 3 How Anticoagulants Work in the Body
- 4 Types of Anticoagulants
- 5 Anticoagulants in Medical Devices
- 6 Applications in Medicine & Diagnostics
- 7 Risks, Side Effects & Safety
- 8 Comparison Table of Different Anticoagulants
- 9 Future of Anticoagulants in Medicine
- 10 FAQs on Anticoagulants
- 11 Wrapping It Up
Introduction to Anticoagulants
Blood clotting, also called coagulation, is one of the body’s defense mechanisms against excessive bleeding. But sometimes, this natural process can backfire. Unnecessary blood clots can form in blood vessels, leading to conditions like stroke, heart attack, and deep vein thrombosis (DVT). To prevent these life-threatening complications, anticoagulants—commonly referred to as “blood thinners”—are used.
But here’s the catch: anticoagulants don’t actually “thin” the blood. Instead, they interfere with the clotting process by targeting clotting factors, enzymes, or pathways in the coagulation cascade. This is the core principle of anticoagulants—managing clotting without completely stopping it.
In addition to clinical treatment, anticoagulants play a vital role in blood collection and diagnostics. For example, SINY Medical’s serum tubes and anticoagulant additives like ACD-A are designed to keep blood samples stable and clot-free, ensuring accurate laboratory results.
Principle of Anticoagulants
The principle of anticoagulants is rooted in one simple idea: interruption of the coagulation cascade.
Blood clotting involves a complex chain reaction where proteins (called clotting factors) activate one another in sequence, forming fibrin that stabilizes a clot. Anticoagulants interfere with different steps in this cascade, such as:
- Blocking vitamin K activity (Warfarin targets this mechanism).
- Inhibiting thrombin (Heparin and direct oral anticoagulants act here).
- Preventing platelet aggregation (Antiplatelet drugs like aspirin).
- Chelating calcium ions (Additives like EDTA in blood tubes bind calcium to prevent clotting).
In essence, anticoagulants ensure that blood either doesn’t clot too quickly inside the body or stays unclotted in test tubes during laboratory analysis.
How Anticoagulants Work in the Body
To understand their mechanism, let’s first explore the clotting cascade:
- Vascular Phase – blood vessels constrict to reduce blood flow.
- Platelet Phase – platelets stick to the damaged area and form a temporary plug.
- Coagulation Phase – clotting factors activate and convert fibrinogen to fibrin.
- Clot Stabilization – fibrin strengthens the clot.
Anticoagulants work by interfering with steps 2–3, either by stopping platelet activity or by preventing clotting factors from being activated.
For example:
- Heparin enhances antithrombin III, which inactivates thrombin.
- Warfarin blocks vitamin K, necessary for clotting factor production.
- Direct oral anticoagulants (DOACs) target specific enzymes like Factor Xa.
Meanwhile, in laboratory use, EDTA or citrate additives in blood collection tubes bind calcium, a key player in the clotting process, ensuring blood remains fluid for testing.
Types of Anticoagulants
Anticoagulants can be classified into clinical drugs (used inside the body) and laboratory additives (used in blood tubes).
1. Heparin
- Fast-acting, injectable.
- Used in surgery and dialysis.
- Prevents thrombin formation.
2. Warfarin (Vitamin K Antagonist)
- Oral anticoagulant.
- Requires regular blood monitoring.
- Used for long-term prevention of clots.
3. Direct Oral Anticoagulants (DOACs)
- Includes apixaban, rivaroxaban, dabigatran.
- Safer with fewer dietary restrictions.
4. Antiplatelet Agents
- Aspirin, clopidogrel.
- Work by preventing platelet clumping.
5. Laboratory Anticoagulants
- EDTA: Common in micro capillary tubes.
- Citrate: Used in coagulation studies.
- ACD-A (Acid Citrate Dextrose): Special additive for PRP tubes.
Anticoagulants in Medical Devices
In diagnostics, anticoagulants are indispensable. Without them, blood collected for testing would clot before analysis, making results invalid.
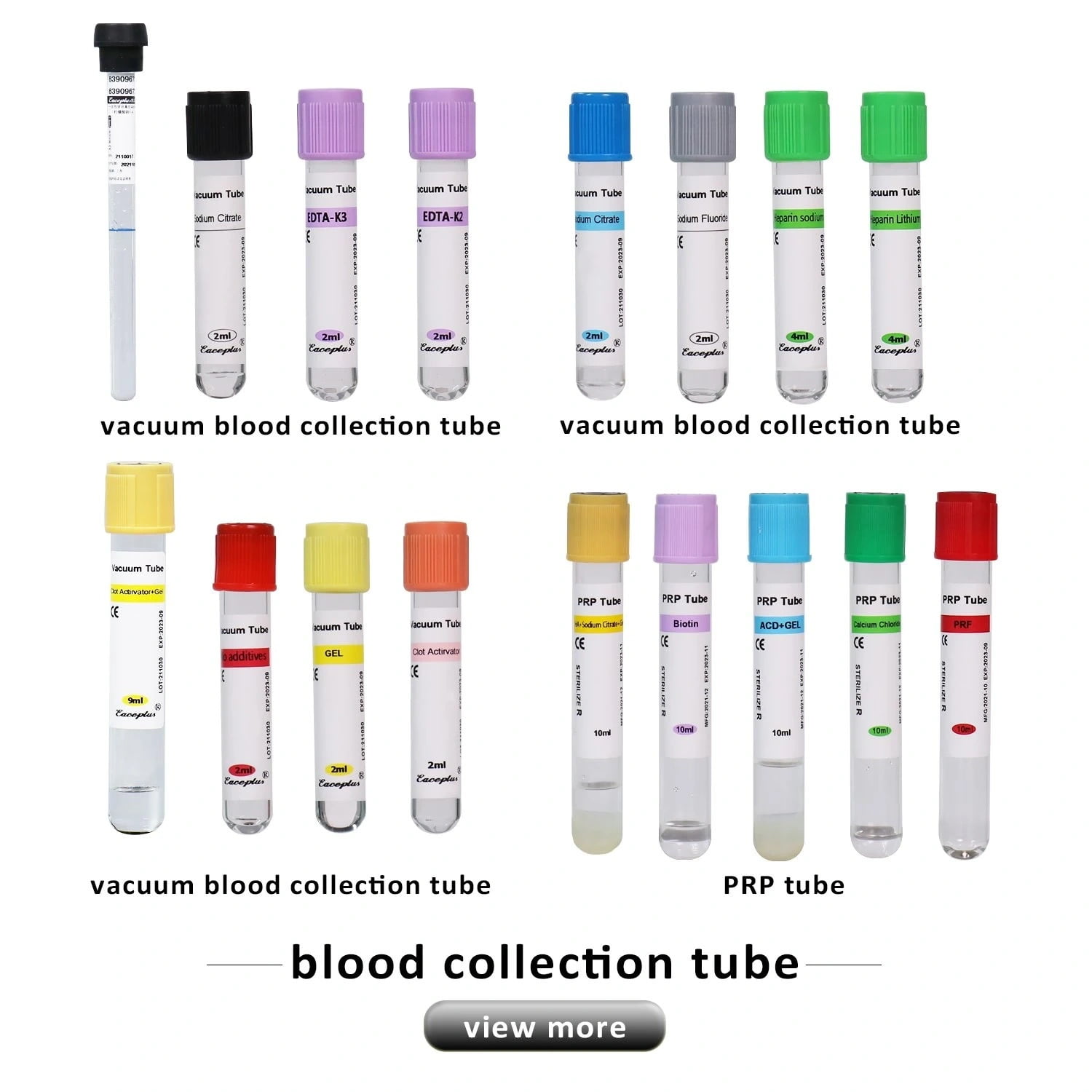
SINY Medical provides a wide range of blood collection tubes with or without anticoagulants:
- Serum Tubes – no anticoagulant, blood is allowed to clot, and serum is collected.
- No Additive Tubes – like the 5ml vacuum blood collection tube.
- Micro Capillary Tubes – used for small-volume collections.
- Red Color No Additive Tube – ideal for biochemical and serological tests.
For more details, you can explore their full product catalog at SINY Medical.
Applications in Medicine & Diagnostics
Anticoagulants are used in:
- Preventing strokes in atrial fibrillation patients.
- Managing deep vein thrombosis and pulmonary embolism.
- During heart surgery and dialysis.
- Laboratory diagnostics where anticoagulants in tubes prevent pre-analysis clotting.
YouTube: SINY Medical even shares educational resources on how their tubes ensure accuracy in lab tests.
Risks, Side Effects & Safety
While anticoagulants save lives, they also carry risks such as:
- Excessive bleeding (gums, nose, internal bleeding).
- Drug interactions (especially with warfarin).
- Dietary restrictions (foods high in vitamin K affect warfarin).
For laboratory use, risks are minimal but choosing the right tube (anticoagulant vs. no additive) is critical for accuracy. Contact SINY Medical for professional guidance.
Comparison Table of Different Anticoagulants
| Anticoagulant | Mechanism | Use | Example Product |
|---|---|---|---|
| Heparin | Enhances antithrombin III | Surgery, dialysis | Injectable only |
| Warfarin | Vitamin K antagonist | Long-term clot prevention | Oral tablets |
| DOACs | Factor Xa / thrombin inhibitors | Stroke prevention | Rivaroxaban, Apixaban |
| EDTA | Chelates calcium | Lab testing | Micro Capillary Tubes |
| Citrate | Calcium binding | Coagulation studies | PRP tubes |
| ACD-A | Preserves blood for PRP | Regenerative medicine | ACD-A PRP Additives |
Future of Anticoagulants in Medicine
Research is focusing on:
- Safer anticoagulants with fewer bleeding risks.
- Targeted therapies for specific clotting factors.
- Improved blood collection devices, like those from SINY Medical, ensuring better accuracy and stability.
FAQs on Anticoagulants
Q1. What is the main principle of anticoagulants?
The principle is to prevent blood from clotting by interfering with clotting factors, enzymes, or calcium.
Q2. Do anticoagulants completely stop clotting?
No, they only slow down clot formation, allowing the body to balance bleeding and clotting safely.
Q3. Which anticoagulant is used in blood collection tubes?
EDTA, citrate, and ACD-A are the most common.
Q4. Are anticoagulants the same as antiplatelets?
No. Antiplatelets prevent platelets from sticking, while anticoagulants act on clotting factors.
Q5. Where can I buy reliable blood collection tubes?
From SINY Medical’s official website.
Wrapping It Up
The principle of anticoagulants lies in their ability to prevent clot formation without completely stopping the body’s protective mechanism. They’re vital in treating cardiovascular diseases, performing surgeries, and ensuring accurate lab diagnostics.
For healthcare providers, laboratories, and researchers, reliable tools matter just as much as reliable drugs. That’s why companies like SINY Medical are leading the way with advanced blood collection tubes, serum tubes, and micro capillary solutions.
For product inquiries or expert guidance, visit SINY Medical’s contact page.