Blood collection is a critical step in medical diagnosis and research. It involves drawing blood samples from patients for analysis in the laboratory. The quality and accuracy of these samples depend on several factors, including the type of blood collection tube used and its additives. Adding clot activators to the tubes used for blood collection can also interfere with downstream immunoassays, thus affecting the results. They play a crucial role in maintaining the integrity of blood samples during transportation, storage, and analysis. This article will explore the different blood collection tube additives types, their functions, and their impact on your samples.
Table of Contents
Types of Blood Collection Tube Additives
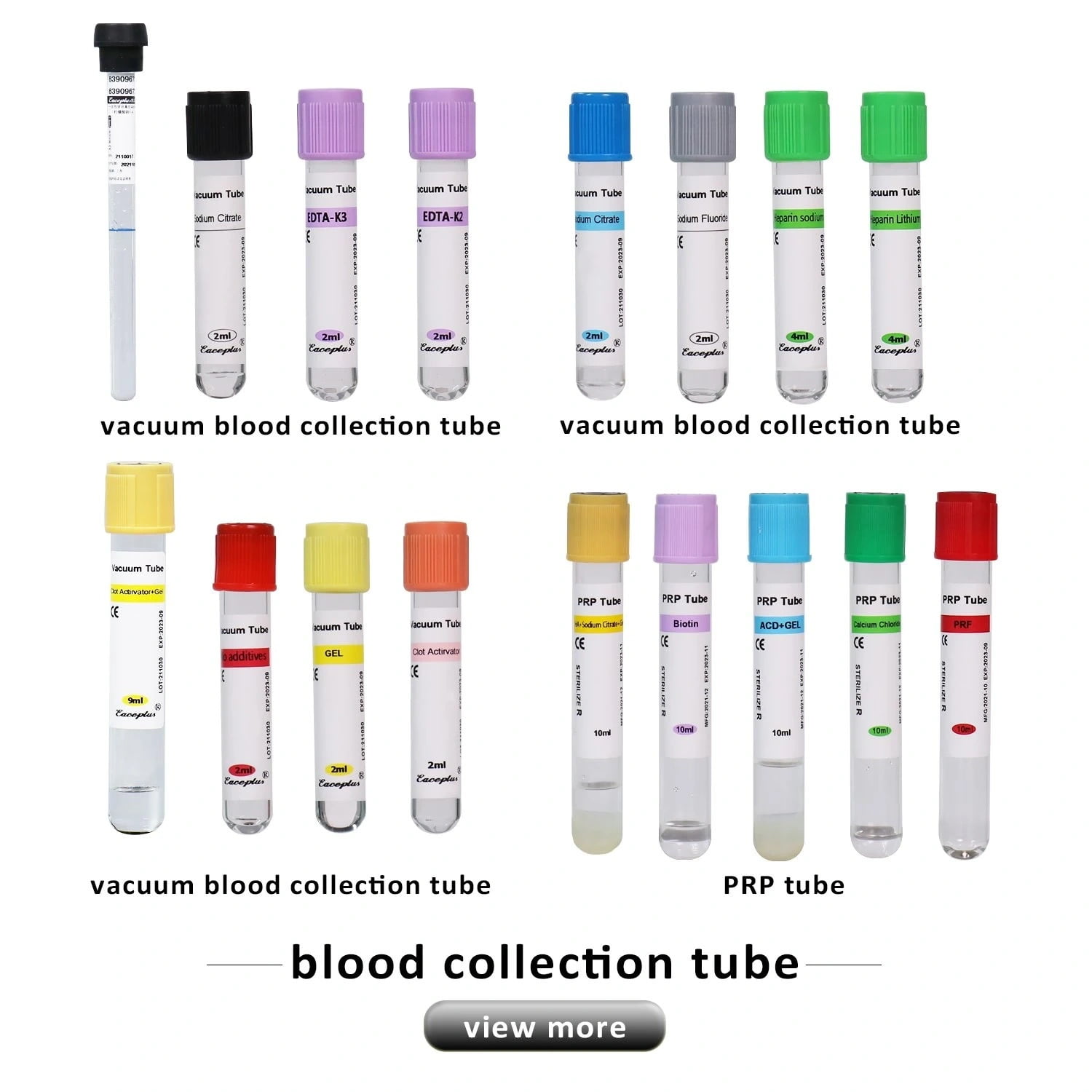
Blood collection tube additives are classified based on their functions and include:
Anticoagulants
Healthcare professionals add anticoagulants to blood collection tubes to prevent blood clotting. They achieve this by inhibiting the clotting factors present in the blood. Anticoagulants are essential in preventing the formation of clots, which can alter the results of laboratory tests. Common anticoagulants used in blood collection tubes include:
- First and foremost, they play a crucial role in obtaining accurate results from blood tests by ensuring that the blood sample remains stable and intact during transportation and testing. Furthermore, they are equally important for maintaining the integrity of the sample. Moreover, they contribute significantly to the reliability of test results. Lastly, blood collection tubes are essential in the field of healthcare.
- EDTA: Ethylenediaminetetraacetic acid (EDTA) is a chelating agent that binds to calcium ions in the blood, which is essential in the clotting process. Healthcare professionals use EDTA in blood collection tubes to prevent clotting, and they commonly use it in hematology tests.
- Sodium Citrate: This is a salt of citric acid that binds to calcium ions in the blood and prevents clotting. Sodium citrate is used in coagulation tests to assess blood clotting ability.
Clot Activators
Healthcare professionals add clot activators to blood collection tubes to enhance blood clotting. They achieve this by activating clotting factors present in the blood. Clot activators are essential in obtaining serum samples from blood. Common clot activators used in blood collection tubes include:
- Healthcare professionals commonly use silica, a finely ground silicon dioxide that activates the clotting factors in the blood, in serum collection tubes.
- Thrombin: This is an enzyme that converts fibrinogen to fibrin, which is essential in the formation of blood clots.Healthcare professionals commonly use thrombin in serum collection tubes.
Preservatives
The manufacturer adds preservatives to blood collection tubes in order to improve sample stability and preservation. They achieve this by preventing the growth of bacteria and other microorganisms in the sample. Common preservatives used in blood collection tubes include:
- Sodium Fluoride: This is a salt of hydrofluoric acid that inhibits the growth of bacteria and prevents the breakdown of glucose in the sample. Healthcare professionals commonly use sodium fluoride in glucose tests.
- Sodium Azide: This is a salt of hydrazoic acid that inhibits bacterial growth in the sample. Healthcare professionals commonly use sodium azide in blood alcohol tests.
- Formaldehyde: This is a solution of formaldehyde gas in water that inhibits the growth of bacteria and preserves the integrity of cellular components in the sample. Healthcare professionals commonly use formaldehyde in cytology tests.
Impact of Blood Collection Tube Additives on Sample Quality
Blood collection tube additives play a crucial role in determining the quality and accuracy of the samples collected. If healthcare professionals add clot activators to the tubes used for blood collection, they can also interfere with downstream immunoassays, thus affecting the results. Here are some ways in which blood collection tube additives affect sample quality:
- The presence of additives can affect laboratory test results.Adding an anticoagulant to a blood collection tube can prevent the blood from clotting, which can lead to errors in the analysis.
- Preservatives and additives can interfere with laboratory test results. An example of this would be the addition of sodium fluoride to a blood collection tube, which can lead to falsely low blood glucose levels.
- For example, formaldehyde, used as a preservative in blood collection tubes, can alter the morphology of cellular components in the sample, making analysis difficult.
- Adding clot activators to the tubes used for blood collection can interfere with downstream immunoassays, thus affecting the results.
FAQs
In healthcare settings, professionals use blood collection tubes to gather and preserve blood samples for different laboratory tests.They come in different types and colors, each containing specific additives designed to preserve the sample’s integrity and ensure accurate test results. In this article, we answer some common questions about blood collection tubes.
Q: What is the difference between a clot activator and an anticoagulant?
A: When blood is drawn into a collection tube, it naturally begins to clot. Clot activators, such as silica or glass particles, promote clotting by providing a surface for clotting factors to interact. On the other hand, anticoagulants, such as heparin or EDTA, prevent blood clotting by inhibiting clotting factors.
Q: Can I use a blood collection tube without additives?
A: No, blood collection tubes without additives can lead to inaccurate test results due to blood clotting.
Q: Can blood collection tube additives affect the quality of DNA samples?
A: Yes, some blood collection tube additives, such as EDTA, can affect the quality of DNA samples by chelating with divalent metal ions required for DNA stabilization. Selecting the appropriate collection tube for DNA testing is important to ensure accurate and reliable results.
Q: How long can blood samples collected in additive-containing tubes be stored?
A: The storage time of blood samples depends on the type of additive present in the tube and the test to be performed. In general, you can store samples collected in anticoagulant-containing tubes for up to 48 hours, and you can store those collected in serum or plasma tubes for up to 72 hours. It is important to follow proper storage protocols to ensure accurate test results.
What are the common types of blood collection tubes?
- Serum tubes: used for tests that require serum, such as chemistry tests.
- Plasma tubes: used for tests that require plasma, such as coagulation tests.
- EDTA tubes: used for tests that require whole blood or plasma for DNA testing or complete blood counts.
- Heparin tubes: used for tests that require plasma, such as electrolyte tests.
- Glucose tubes: used for glucose tests.
- Blood culture tubes: used for microbiological tests.
Q: How do I choose the right blood collection tube for my test?
A: The selection of the appropriate blood collection tube depends on the type of test being performed. It is important to consult with the laboratory or healthcare provider to determine the correct tube to use for the specific test.
Q: What is the correct way to handle blood collection tubes?
A: Blood collection tubes should be handled carefully to ensure accurate test results. Some tips include:
- Store tubes at the recommended temperature and avoid exposure to light.
- Use tubes within their expiration date.
- Gently invert tubes to mix additives with blood.
- Label tubes with patient information and test type.
- Transport tubes to the laboratory as soon as possible.
Q: Can I reuse blood collection tubes?
A: Blood collection tubes are designed for single use only and should be properly disposed of afterward. Reusing tubes can lead to contamination and inaccurate test results.
Q: What are the risks associated with blood collection?
A: Blood collection is generally considered safe, but there are some risks associated with the procedure. These include:
- Pain or discomfort at the puncture site.
- Bleeding or bruising at the puncture site.
- Infection at the puncture site.
- Fainting or dizziness.
It is important to follow proper infection control protocols and use sterile equipment to minimize the risk of infection.
Conclusion
Blood collection tube additives are essential components of blood collection tubes. They play a crucial role in obtaining accurate results from blood tests by ensuring that the blood sample remains stable and intact during transportation and testing. Furthermore, they are equally important for maintaining the integrity of the sample. Moreover, the designers have designed blood collection tubes with features like leak-proof construction and proper labeling, further enhancing their significance in the process. Additionally, healthcare professionals find them convenient for efficiently collecting blood samples. Lastly, they contribute significantly to the reliability of test results, making them a fundamental aspect of modern medical diagnostics.