Hemoglobin A1c (HbA1c) testing is a cornerstone in diabetes diagnosis and management, offering a reliable measure of average blood glucose levels over the past 8 to 12 weeks. Unlike single-point blood glucose tests, HbA1c provides a comprehensive view of long-term glycemic control, making it indispensable for healthcare providers and patients. However, the accuracy of HbA1c results hinges on several factors, with the choice of blood collection tubes being one of the most critical. Using the wrong tube can compromise test results, leading to misdiagnosis or improper treatment plans. In this in-depth guide, we’ll explore the types of blood collection tubes suitable for HbA1c testing, why they matter, and best practices for ensuring reliable results.
Table of Contents
Why HbA1c Testing Requires Specific Blood Collection Tubes
HbA1c testing measures the percentage of hemoglobin in red blood cells that has glucose attached to it. This process requires whole blood samples containing intact red blood cells, as hemoglobin resides within these cells. Using inappropriate tubes, such as those designed for serum or plasma collection, can damage or remove red blood cells, rendering the sample unsuitable for analysis. The right blood collection tubes ensure the sample remains stable, anticoagulated, and compatible with HbA1c analyzers, preserving the integrity of red blood cells for accurate results.
Tubes with additives like clot activators or separation gels are designed to isolate serum or plasma, which eliminates the red blood cells needed for HbA1c measurement. Similarly, tubes with anticoagulants unsuitable for HbA1c testing can interfere with analytical methods, such as high-performance liquid chromatography (HPLC) or immunoassays.
The Gold Standard — EDTA Blood Collection Tubes
When it comes to HbA1c testing, EDTA tubes are the undisputed winner. They contain Ethylenediaminetetraacetic acid (EDTA) — an anticoagulant that binds calcium ions, preventing blood from clotting while preserving cell shape and structure.
You can explore the different EDTA tubes offered by Siny Medical for laboratory use.
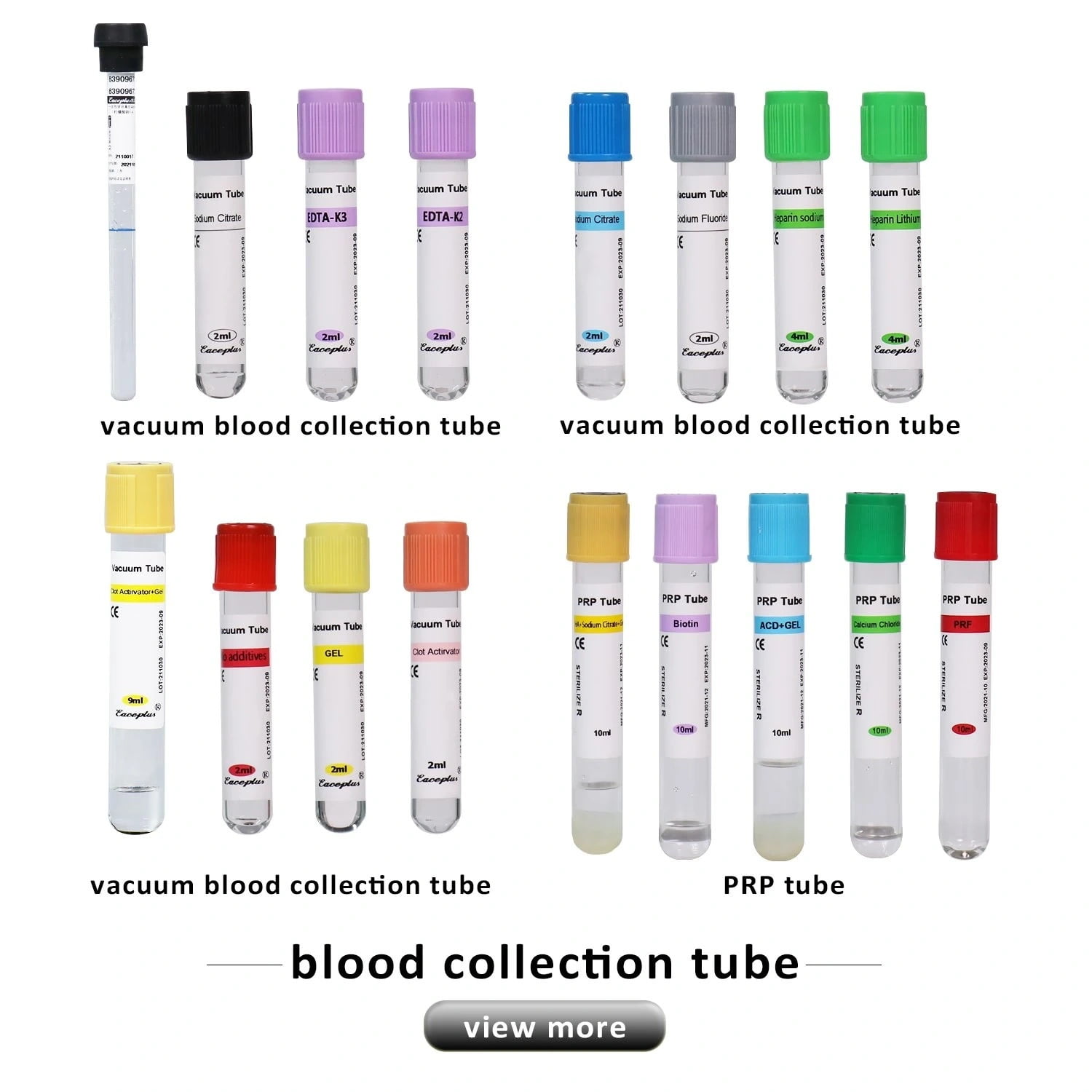
Types of EDTA Tubes Commonly Used for HbA1c
- K2 EDTA (Dry Additive) Lavender-Top Vacuum Tubes
- Contain potassium salt of EDTA in dry form.
- Gentler on red cell morphology, making them ideal for automated HbA1c analyzers.
- Widely preferred in modern labs.
- K3 EDTA (Liquid Additive) Lavender-Top Vacuum Tubes
- Contain EDTA in liquid form.
- Still effective, but may slightly alter red cell size and shape in some cases.
- Used in certain older or specific analyzer systems.
- Non-Vacuum EDTA Tubes
- Often used in small clinics or manual collection settings.
- Require careful handling to avoid contamination or incorrect blood-to-anticoagulant ratios.
Why EDTA?
- Prevents blood clotting by binding calcium
- Maintains RBC integrity for accurate HbA1c measurement
- Compatible with HPLC, immunoassay, and enzymatic HbA1c metho
For a deeper look at why EDTA tubes are recommended, check this research-backed resource: Why EDTA Tubes Are Preferred for HbA1c Test.
Why Other Blood Collection Tubes Are Not Suitable for HbA1c
It’s tempting to think that any tube will do — but here’s why that’s risky:
- Heparin Tubes (Green Cap)
- Intended for plasma-based tests.
- May interfere with High-Performance Liquid Chromatography (HPLC) — one of the most common HbA1c methods.
- Sodium Citrate Tubes (Blue Cap)
- Used for coagulation studies, not chemistry.
- Dilutes the blood, which can artificially lower HbA1c results.
- Clot Activator + Gel Tubes
- Designed for serum separation.
- The gel barrier removes RBCs, making the sample unusable for HbA1c.
- Sodium Fluoride/Potassium Oxalate Tubes
- Used for glucose preservation in plasma.
- They prevent glycolysis but are not compatible with HbA1c analysis methods.
- No Additive Tubes
- These allow blood to clot, making them useless for HbA1c, which requires unclotted whole blood.
Practices for Collecting and Handling HbA1c Samples
To ensure accurate HbA1c results, follow these guidelines:
- Fill the Tube Completely
- Underfilling alters the anticoagulant-to-blood ratio, leading to clotting.
- Mix Gently (8-10 Inversions)
- Ensures proper anticoagulation without hemolysis.
- Store at 2–8°C if Testing is Delayed
- Samples remain stable for up to 7 days when refrigerated.
- Avoid Freeze-Thaw Cycles
- Freezing whole blood can rupture RBCs, skewing results.
- Use Within 48 Hours for Best Accuracy
- Prolonged storage may degrade hemoglobin.
For more details, check our blood collection tubes guide.
Final Takeaway
When it comes to HbA1c testing, not all blood collection tubes are created equal. For reliable, reproducible results, K2 or K3 EDTA tubes remain the gold standard. Avoid tubes with gel, clot activators, sodium citrate, or heparin, as they can compromise your sample.
By using the right tube, following best handling practices, and sourcing from trusted suppliers like Siny Medical, you can ensure that every HbA1c result is accurate — supporting better diabetes diagnosis, monitoring, and patient care.
FAQs
Can I use heparin tubes for HbA1c testing?
No — heparin can interfere with certain HbA1c testing methods like HPLC, leading to unreliable results.
Is fasting required before HbA1c testing?
Not at all — HbA1c reflects long-term glucose control, not short-term fluctuations.
How long can I store a blood sample for HbA1c?
Up to 7 days at 2–8°C. For longer storage, freeze it — but avoid repeated freeze-thaw cycles.
Is K2 EDTA more accurate than K3?
Both work well, but K2 EDTA generally preserves cell shape better and is preferred in most labs.
Q5. Why is whole blood necessary for HbA1c?
Because HbA1c is inside red blood cells — without them, you can’t measure it accurately.